-
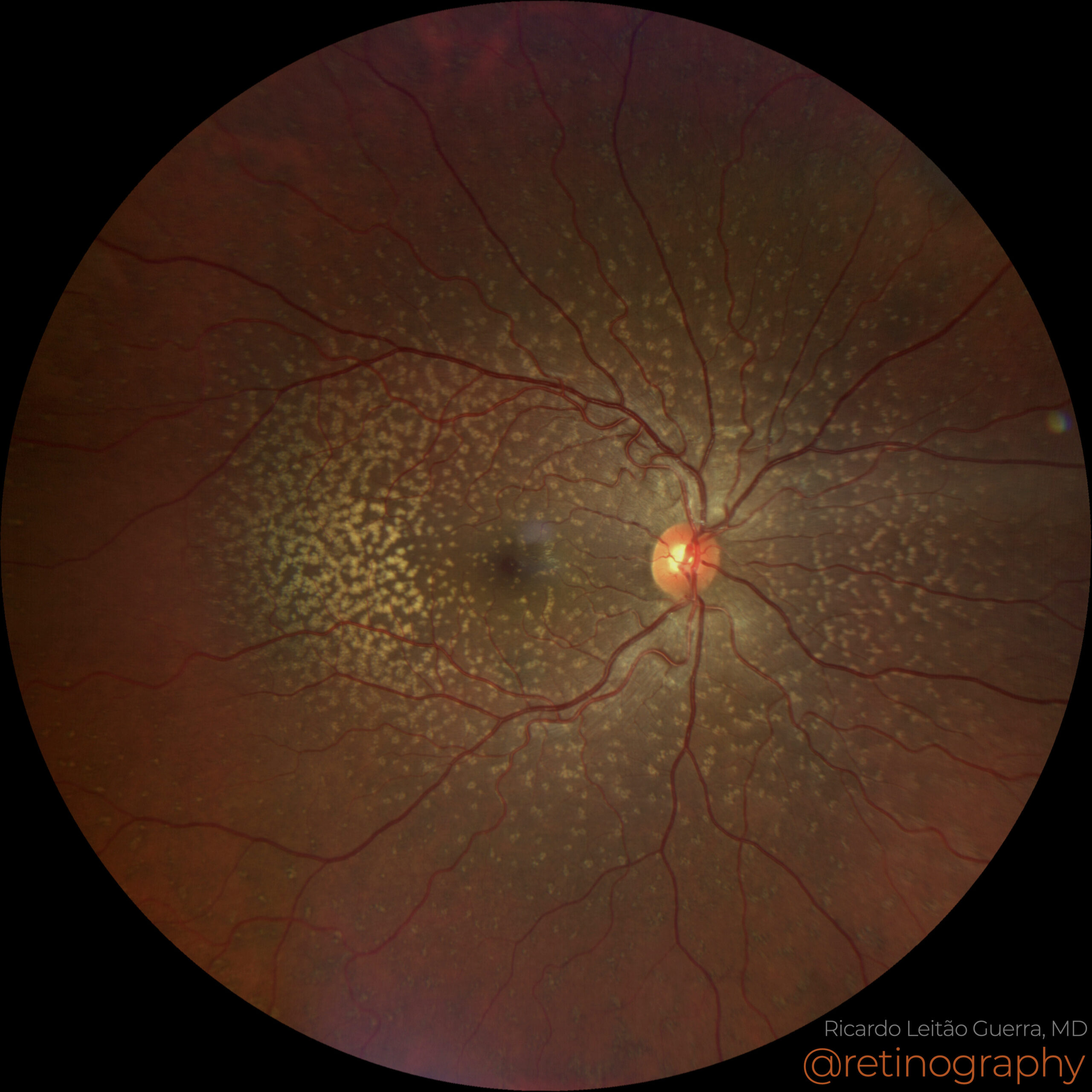
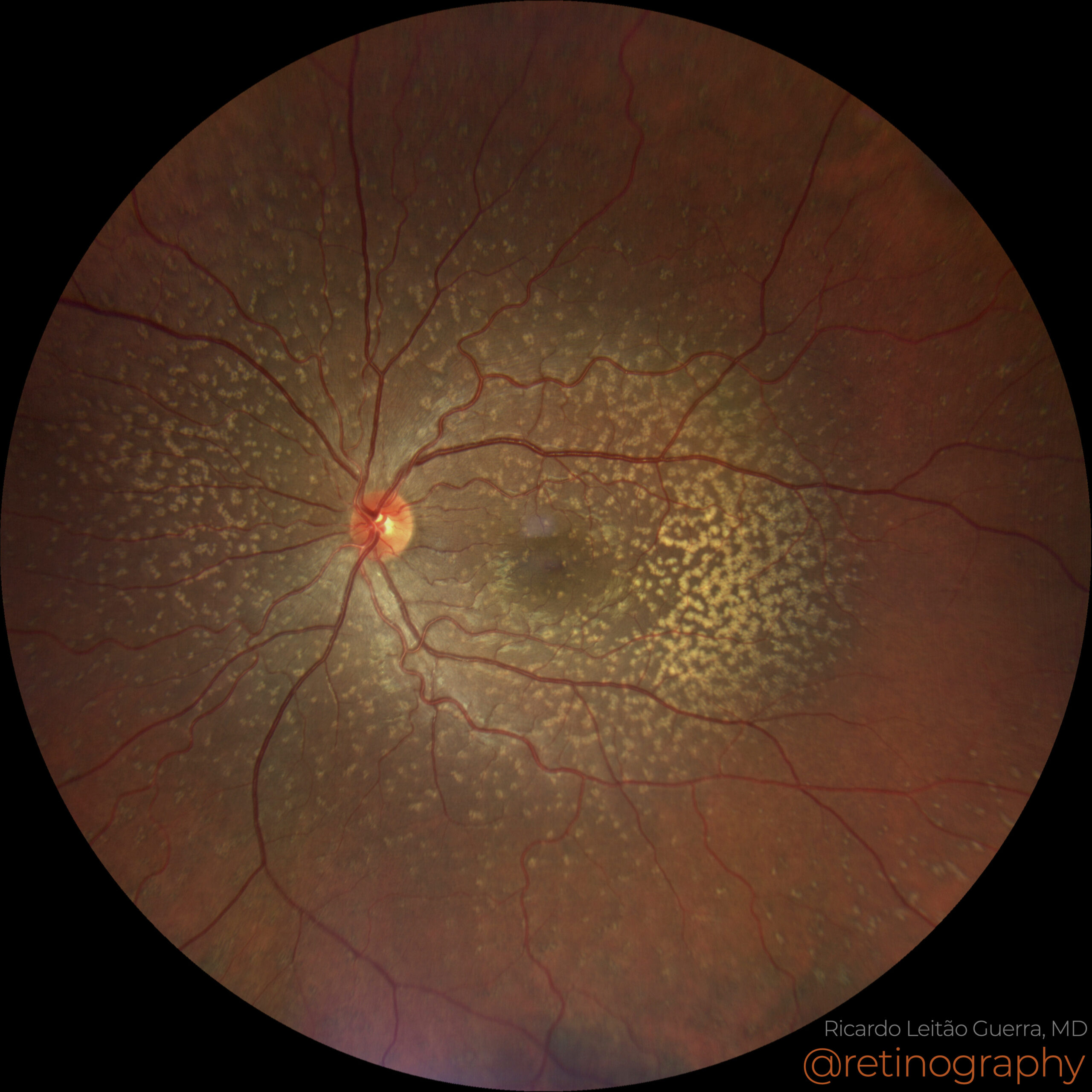
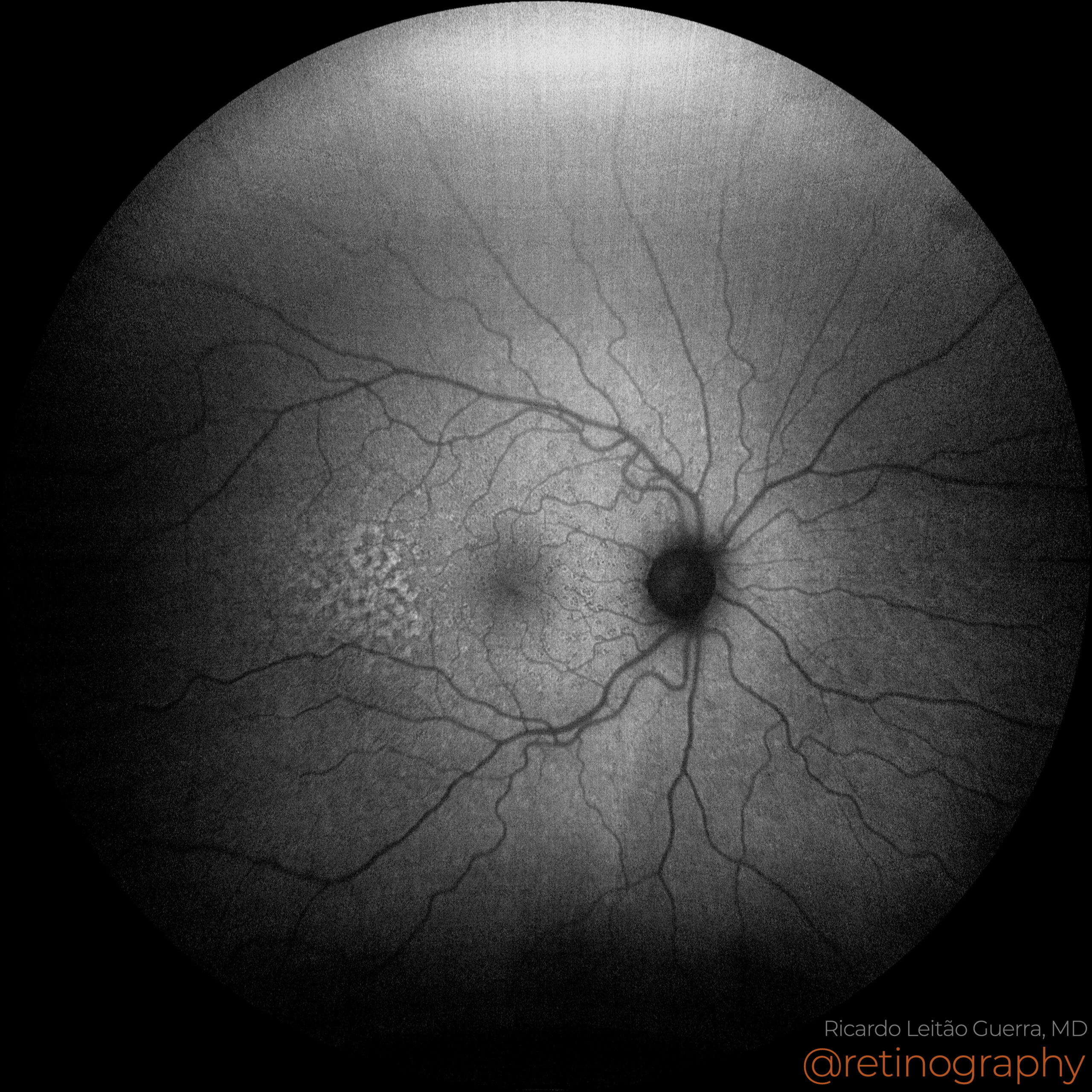
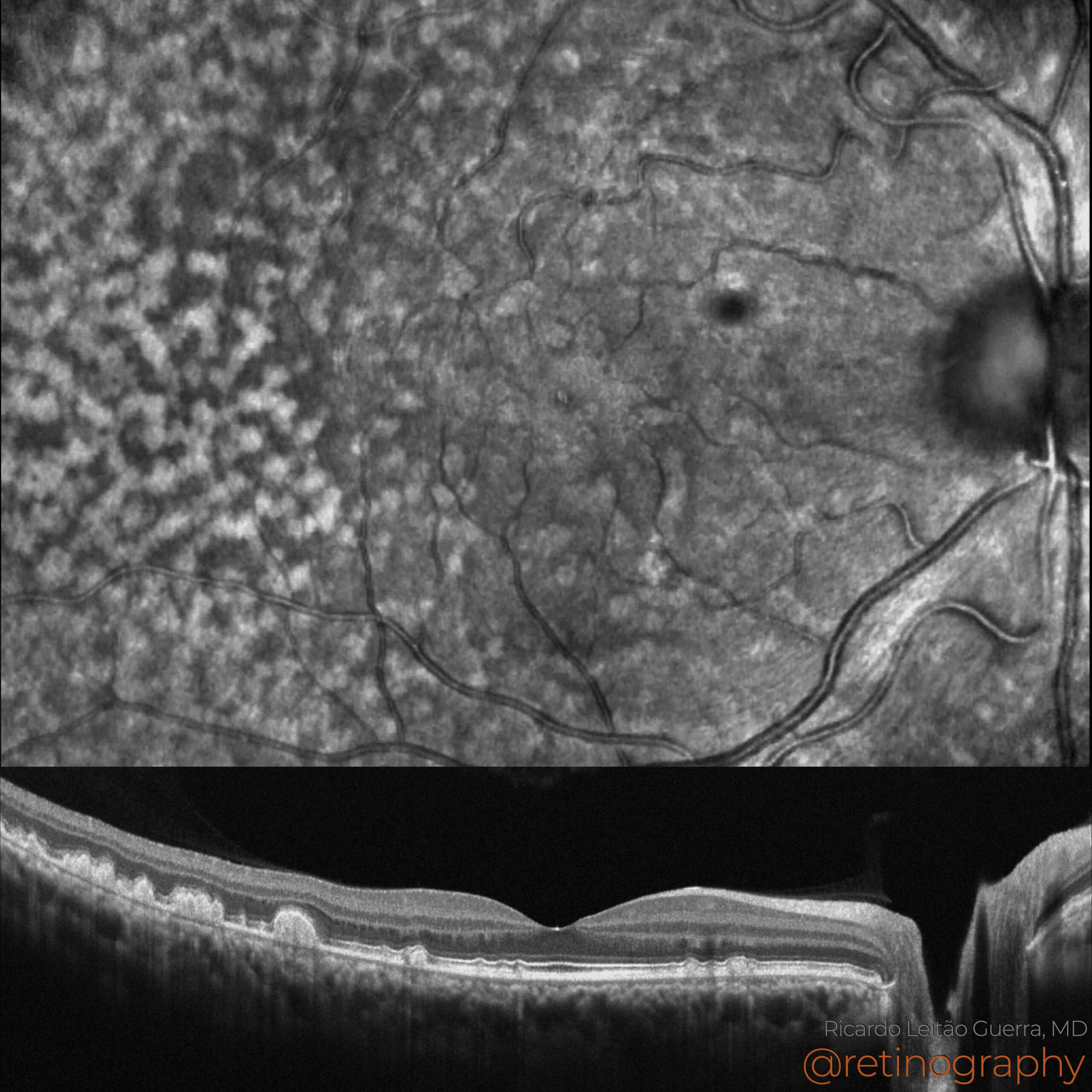
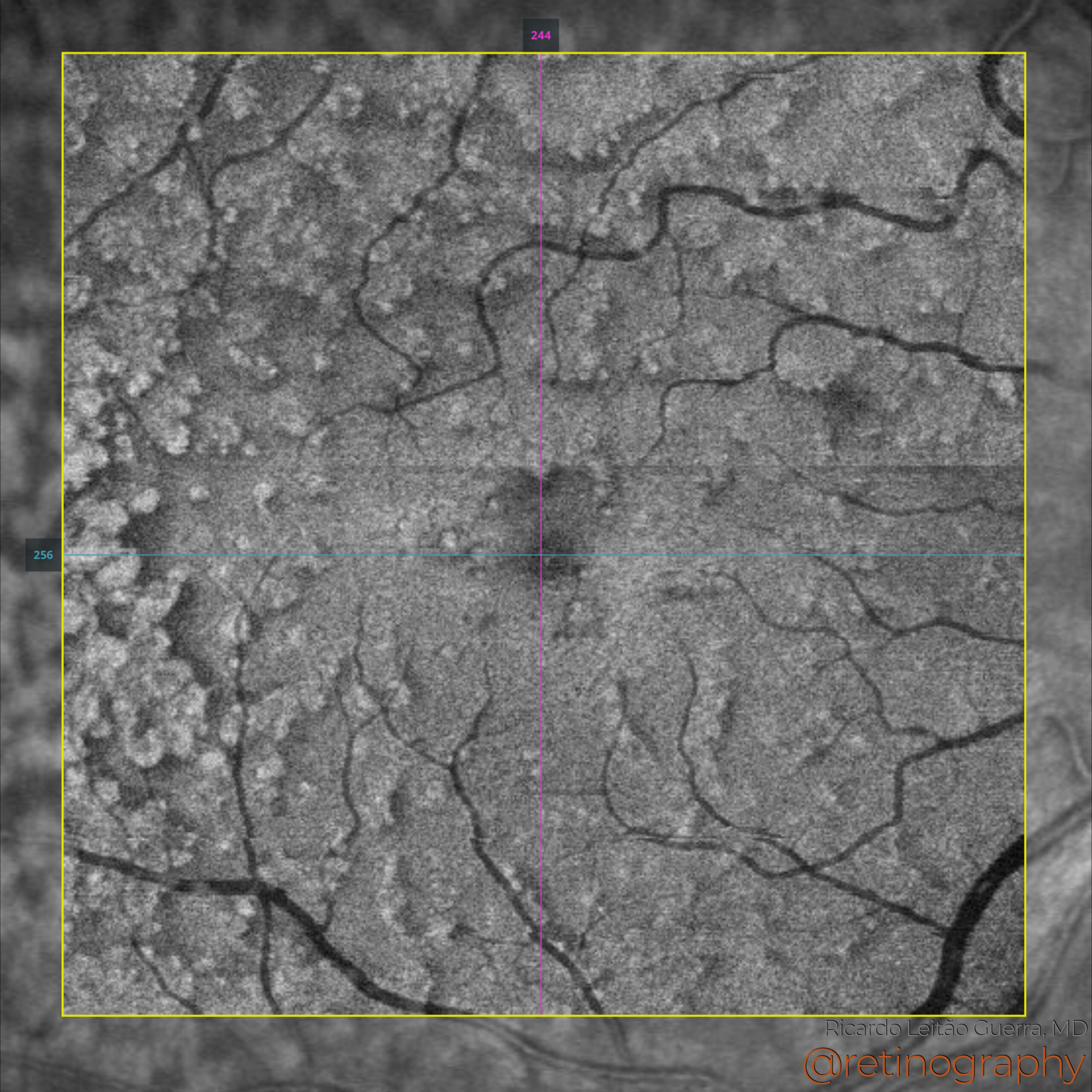
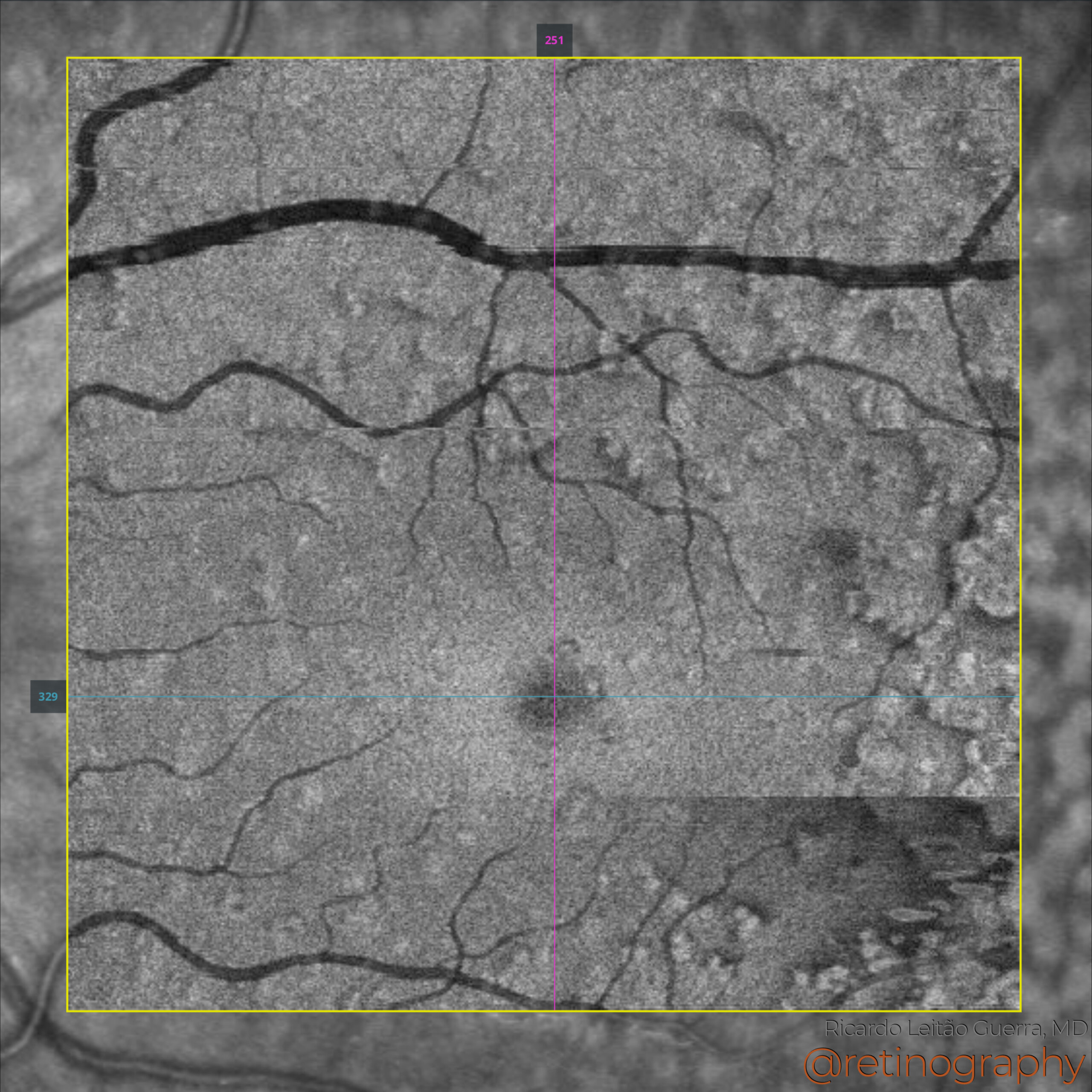
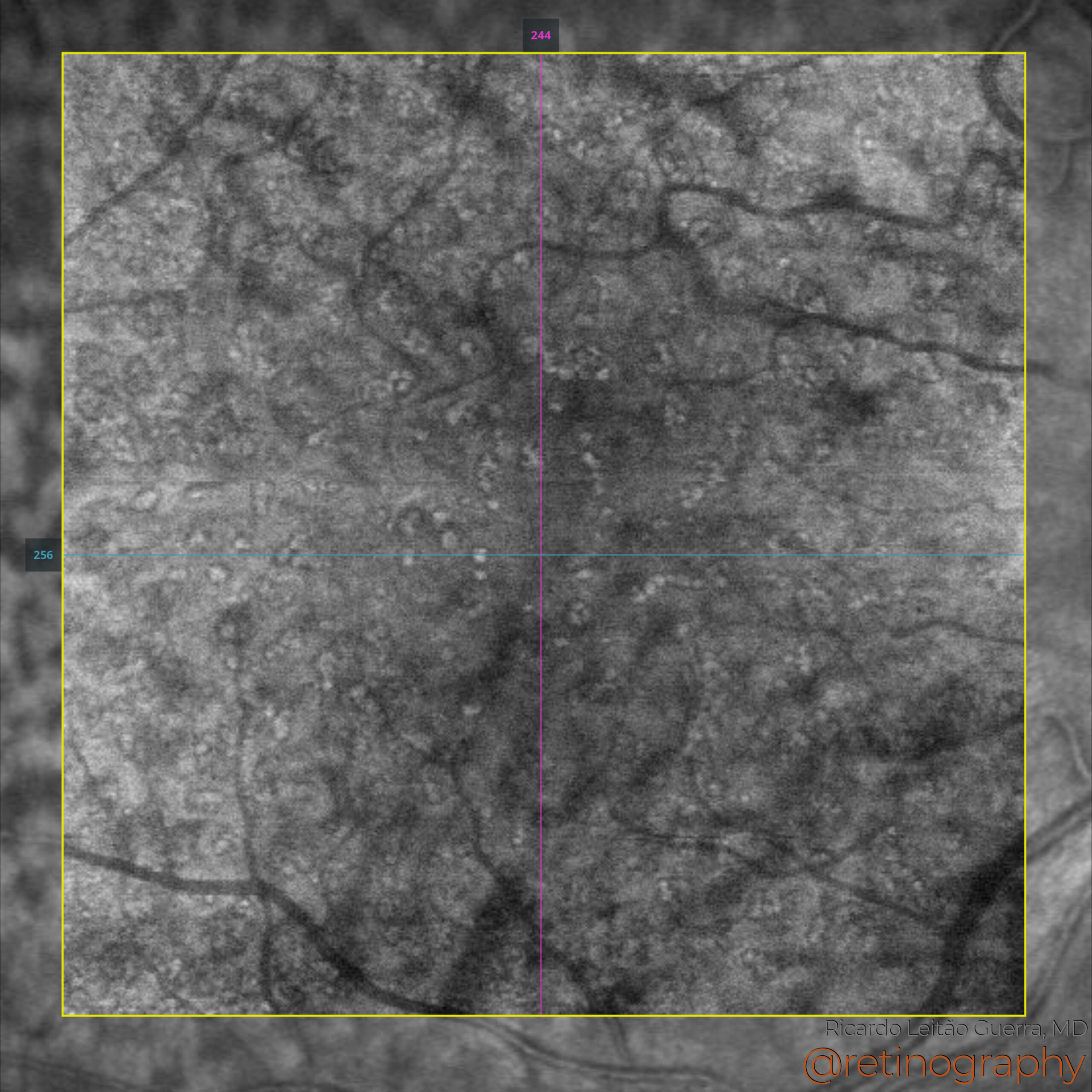
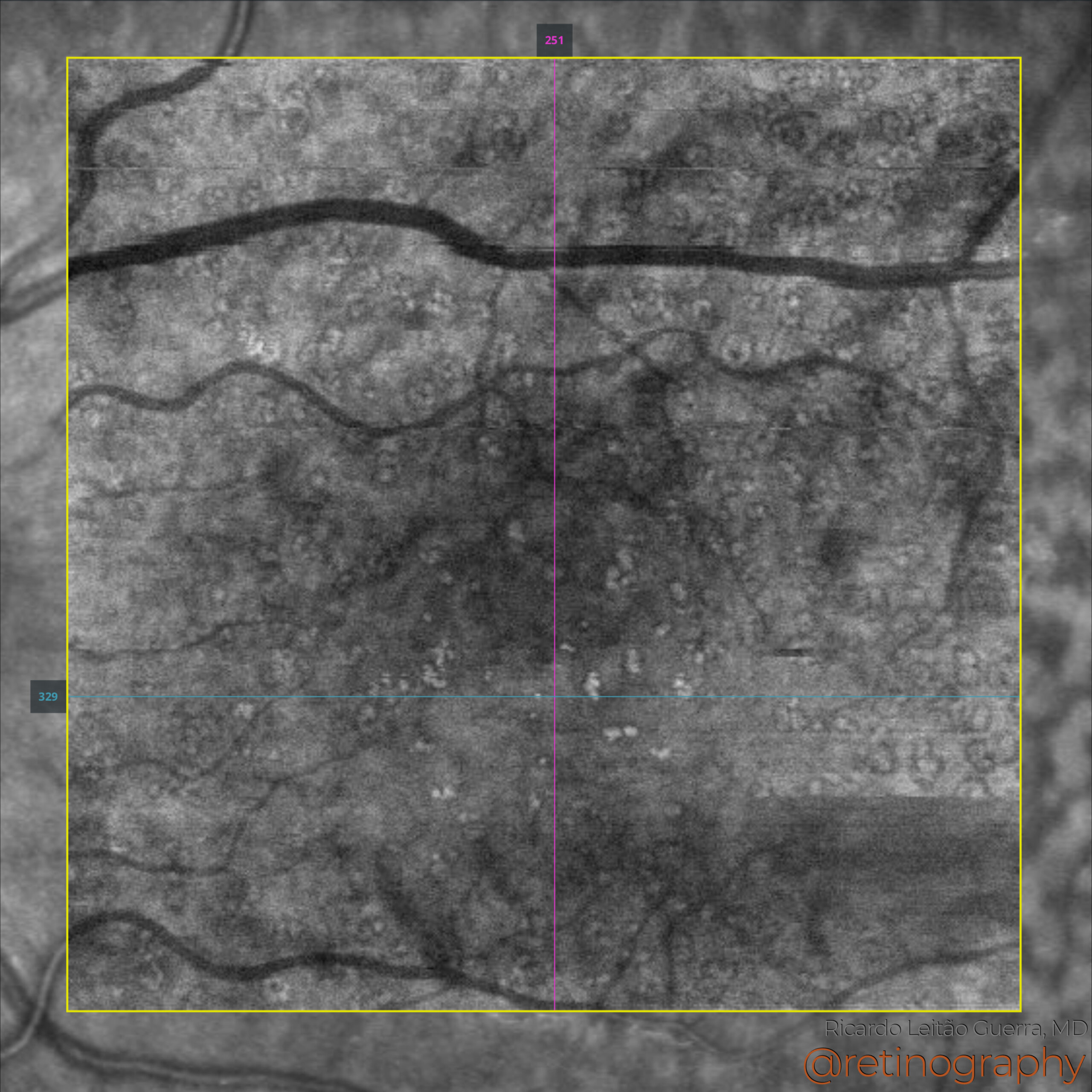
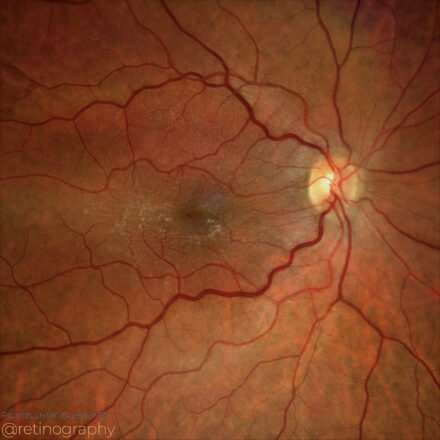
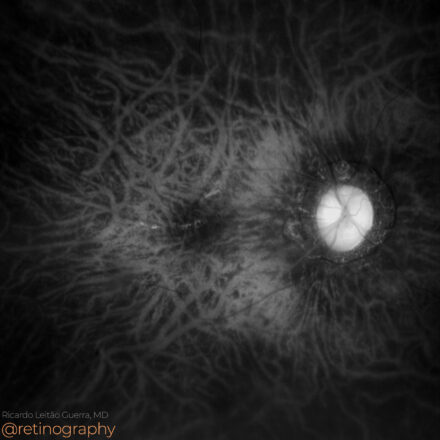
Cuticular Drusen
 32yo
32yo Cuticular drusen, also known as basal laminar drusen, are small, round yellow deposits beneath the retina, often clustered. They are visible in early adulthood and can be mistaken for age-related macular degeneration (AMD). Imaging techniques like OCT and fluorescein angiography are crucial for accurate diagnosis and monitoring. In the context of OCT imaging, hyper transmission is a notable finding often associated with cuticular drusen. This occurs due to the characteristics of the drusen themselves and their effects on the underlying structures: Cuticular drusen can cause attenuation or thinning of the RPE layer, which in turn permits greater transmission of the OCT light. This hypertransmission signal helps to distinguish these drusen from other types that may be characterized by less light penetration due to denser material or thicker RPE disruption.
Disclosure: All images featured in this post were acquired and analyzed using devices integrated within the Zeiss Retina Workflow. This ensures high-quality, detailed visual data for comprehensive assessment.
Other Cases
-
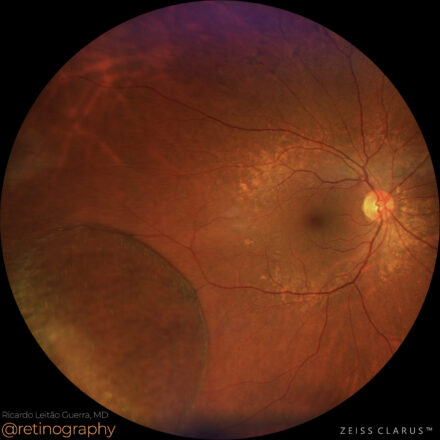
Sickle cell retinopathy
 15yo
15yo In sickle cell retinopathy, peripheral ischemia occurs due to the occlusion of small retinal blood vessels by sickle-shaped red blood cells, which have decreased flexibility and increased adhesion to vascular endothelium. These blockages cause oxygen deprivation in the peripheral retina, leading to tissue hypoxia, neovascularization (e.g., sea fan formations), and […]
-
Diabetic retinopathy: ERM following PRP
 79yo
79yo In proliferative diabetic retinopathy (PDR), panretinal photocoagulation (PRP) is a standard treatment to reduce neovascularization and prevent vision loss. However, PRP may contribute to the formation of an epiretinal membrane (ERM) due to retinal inflammation and scarring. ERM can cause visual distortion and may require surgical peeling if it significantly […]
-
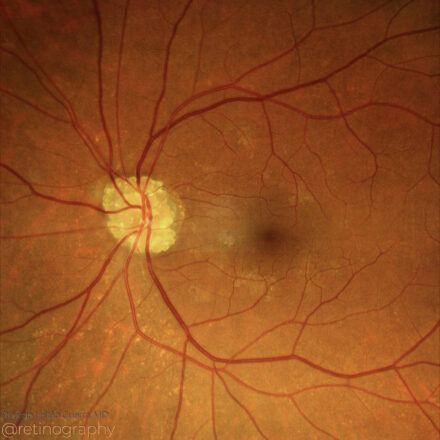
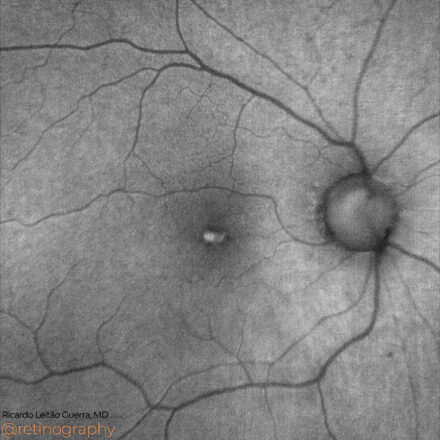
Optic disc drusen
 64yo
64yo Optic disc drusen appear as small, yellowish deposits within the optic nerve head and are visible on fundus examination, often with a lumpy or irregular appearance. These drusen can sometimes simulate optic disc edema, so accurate identification is essential. They may increase the risk of visual field defects and require […]
-
Epiretinal membrane
 70yo
70yo An epiretinal membrane (ERM) is a thin, fibrous layer that forms on the inner retinal surface, causing visual distortion and blurriness. Optical Coherence Tomography (OCT) shows ERM as a hyperreflective layer on the retina’s inner surface, often with retinal thickening and distortion. Treatment may involve observation or surgical removal (membrane […]
-
Peripheral retinoschisis
 69
69 Peripheral retinoschisis is a splitting of the retinal layers that can be mistaken for retinal detachment due to similar fundoscopic appearance. However, retinoschisis is generally more stable and lacks the subretinal fluid that characterizes a true detachment. Optical Coherence Tomography (OCT) and careful clinical examination help distinguish between the two, […]
-
Degenerative myopia: Tessellated fundus
 40
40 In degenerative myopia, a tessellated (or tigroid) fundus appears due to thinning of the retinal pigment epithelium (RPE), which reveals the underlying choroidal vasculature as a mosaic pattern. Red channel imaging enhances the contrast of this pattern, providing clear visualization of these structural changes. #DegenerativeMyopia #TessellatedFundus #RedChannel #RetinaImaging #ChoroidalVasculature #retina […]
-
Diabetic macular edema
 79yo
79yo Diabetic macular edema (DME) is characterized by retinal thickening and fluid accumulation in the macula, often leading to vision loss. Fluorescein angiography (FA) is crucial for evaluating DME, as it reveals areas of capillary leakage, microaneurysms, and zones of ischemia. This imaging helps to assess the extent of vascular damage, […]
-
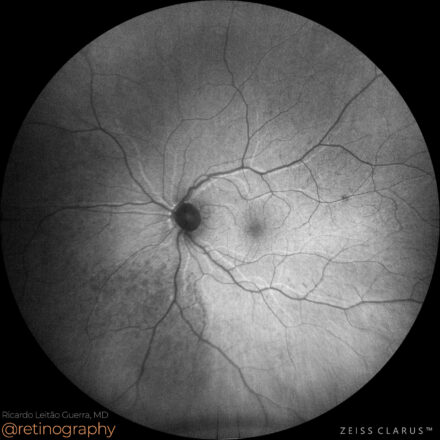
AMD: Geographic atrophy
 89
89 In age-related macular degeneration (AMD) with geographic atrophy, fundus autofluorescence (FAF) is used to assess the extent of retinal pigment epithelium (RPE) loss. Areas of atrophy appear as hypoautofluorescent zones due to the absence of RPE, while hyperautofluorescent borders may indicate regions at risk for progression. FAF is essential for […]
-
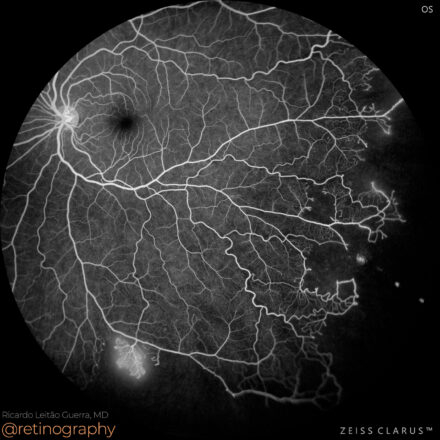
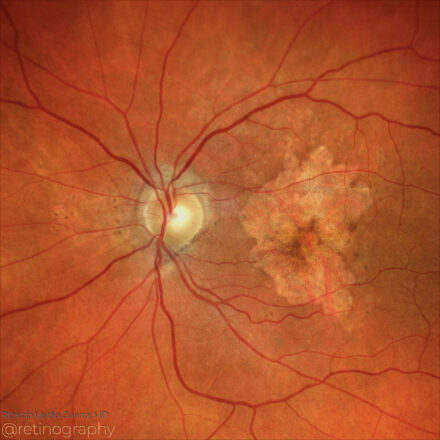
Proliferative Sickle cell retinopathy
 15
15 In proliferative sickle cell retinopathy, fluorescein angiography (FA) is crucial for identifying areas of peripheral ischemia and neovascularization, particularly the characteristic “sea fan” neovascular formations. FA highlights areas of non-perfusion and leakage, helping to map the extent of ischemia and guide interventions such as laser photocoagulation to prevent complications like […]
-
Acquired Vitelliform Lesion
 80yo
80yo Acquired Vitelliform Lesions (AVL) are characterized by subretinal yellowish deposits that can be assessed using multimodal imaging. Fundus autofluorescence (FAF) shows hyperautofluorescence in the area of the lesion due to lipofuscin accumulation. Optical Coherence Tomography (OCT) reveals these deposits as hyperreflective material between the retinal pigment epithelium (RPE) and photoreceptors, […]
-
Degenerative myopia: Lacker cracks
 40
40 In degenerative myopia, lacquer cracks are breaks in Bruch’s membrane that appear as fine, yellowish lines in the posterior pole. These cracks are caused by excessive axial elongation and can lead to complications such as choroidal neovascularization. Fundus imaging helps detect these characteristic lesions, essential for monitoring progression and assessing […]
-
Low-integrity retinal attachment
 65
65 Retinal reattachment in the wrong position can occur following surgery for retinal detachment, and fundus autofluorescence (FAF) can reveal hyperautofluorescent lines where the retinal vessels originally lay. These lines represent areas of misalignment and retinal pigment epithelium (RPE) stress, providing insight into the surgical outcome and potential functional impact. #RetinalReattachment […]